Events
Hosted Events
View all hosted events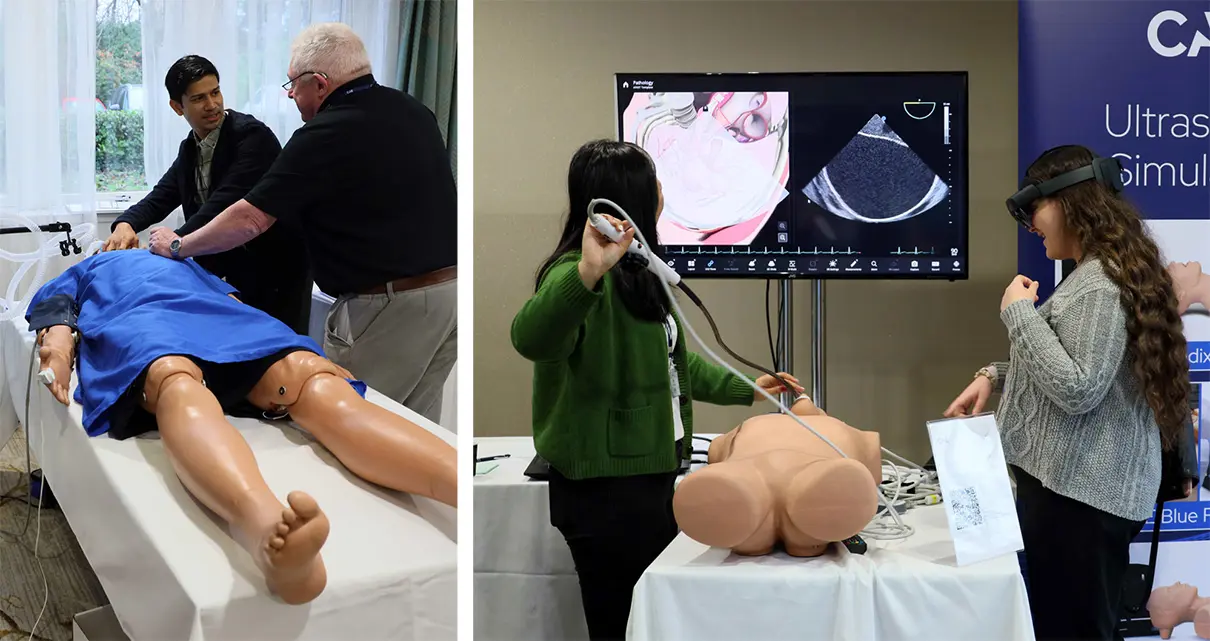
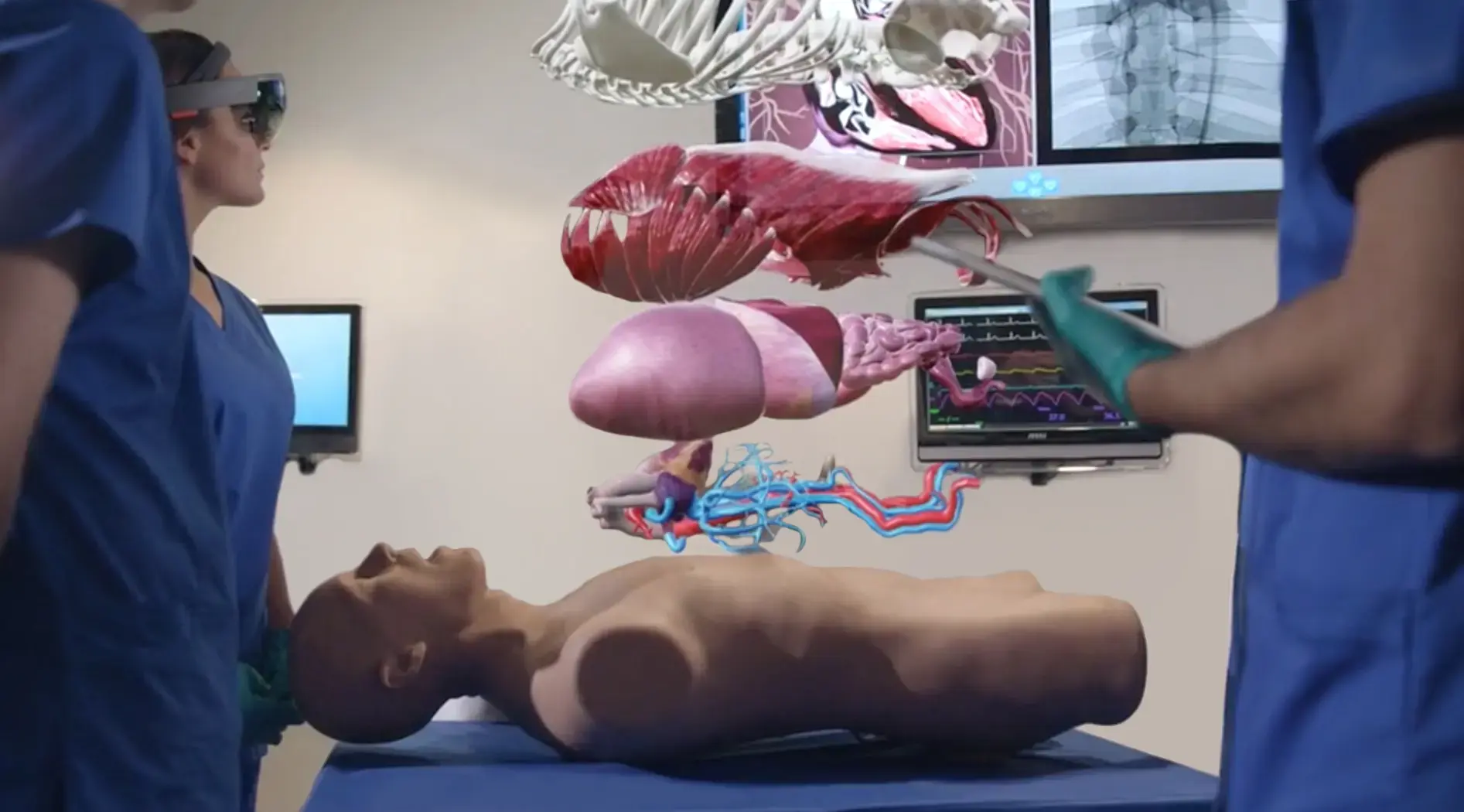
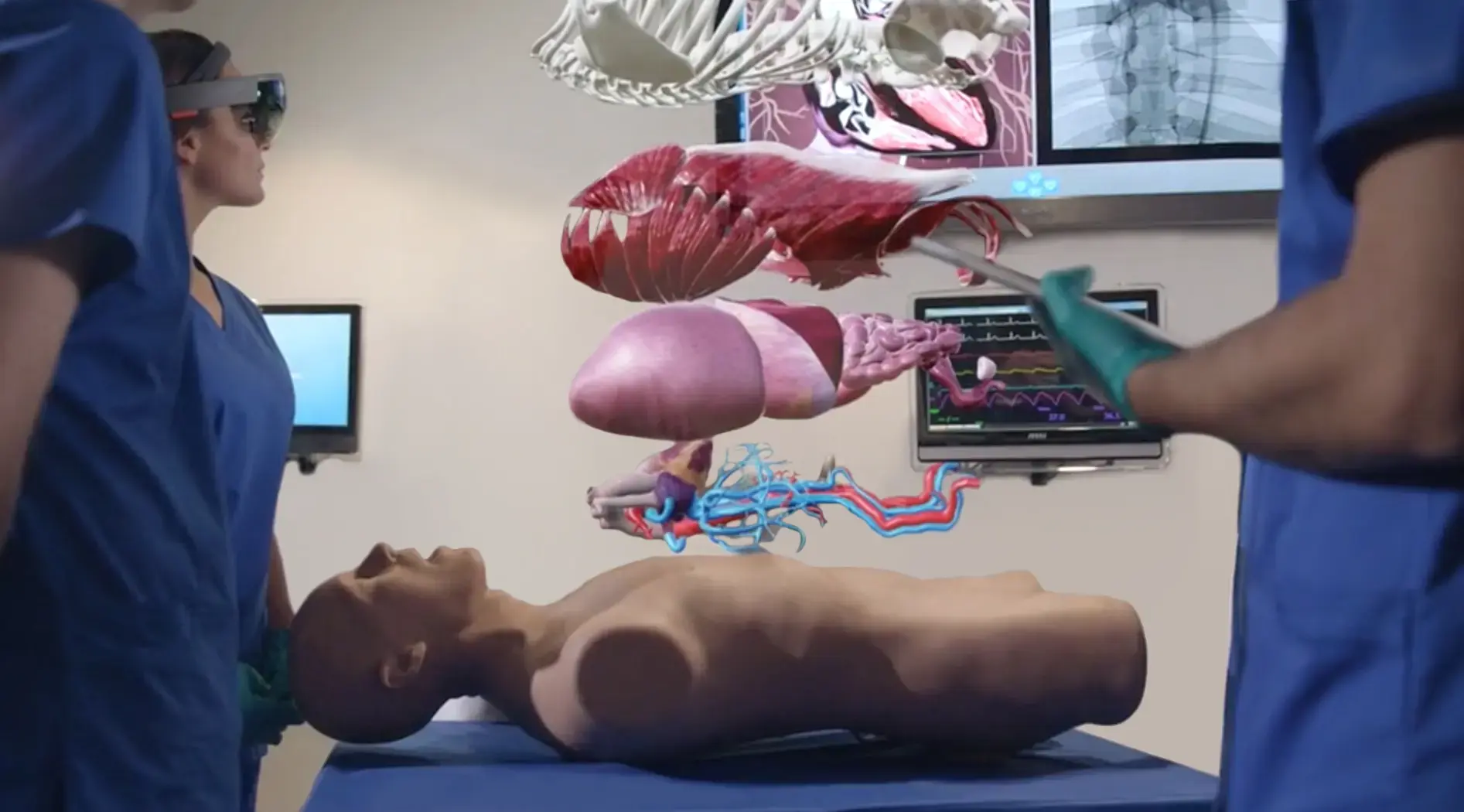
HPSN Deutschland 2024
Der HPSN (Human Patient Simulator Network) ist ein Kongress rund um das Thema Praxis und Innovation in der medizinischen Simulation für Ausbilder, Professoren, Ärzte, Techniker, Pflege- und
Hebammenverantwortliche, Notfallmediziner und alle mit der Sicherheit und Ausbildung in der medizinischen Gesundheitsversorgung betraut sind. Knüpfen Sie wertvolle Kontakte, lernen Sie von Fachvorträgen und beteiligen Sie sich an den Workshops. Wir freuen uns auf Ihren Besuch.
The Human Patient Simulator network Germany (HPSN) is a conference focused on advancing the practice and innovation of healthcare simulation for educators, technologists, technicians, nurses, doctors, midwives, allied health, patient safety leads and other healthcare professionals. Join us in Mainz to experience the technology behind simulation in healthcare education and its application in all care settings. We are looking forward to meet you there.
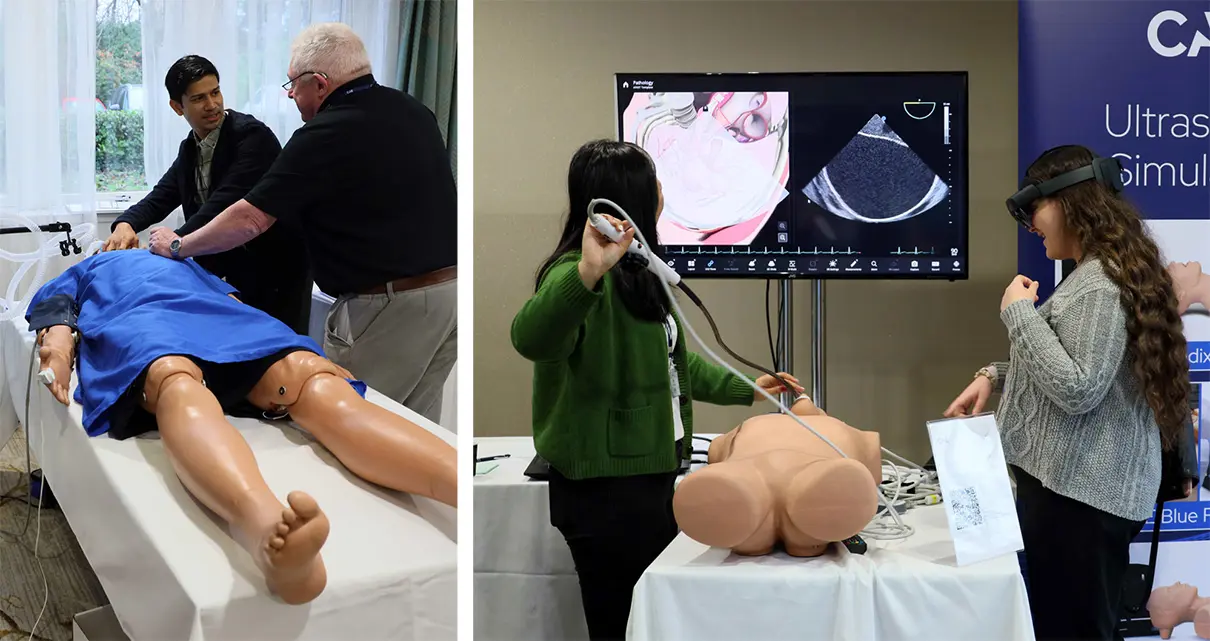
HPSN UK & Ireland 2024
The Human Patient Simulator Network (HPSN) is a conference focused on advancing the practice and innovation of healthcare simulation for educators, technologists, technicians, nurses, doctors, midwives, allied health, patient safety leads and other healthcare professionals. Join us in Coventry to experience the technology behind simulation in healthcare education and its application in all care settings. We are looking forward to meet you there.



